CD96 is a receptor protein on the surface of two types of immune cells: natural killer cells and killer T cells.
They are responsible for continuously screening our bodies for foreign invaders.
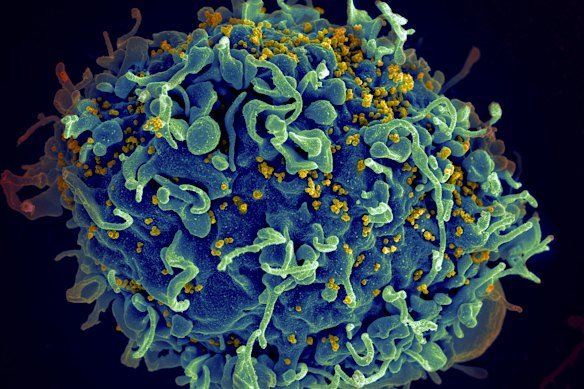
This electron microscope image shows a human T cell, in blue.Credit: NIH/AP
Killer T cells typically reside in our lymph nodes (in the neck and armpits; they swell when we get sick) and spleen. Our lymphatic system can be seen as our body’s sewer piping – if there’s a foreign invader, it will show up here sooner or later.
T cells have a main receptor that can sense foreign nasties, plus lots of secondary receptors. When the main receptors get a hit, they massively multiply and leave the sewers to attack the invader.
“Everything is about shape with this,” said one immunologist, speaking anonymously to discuss the Smyth matter. “Each of your T cell receptors, you’ve just got this massive amount of diversity on what they look like. So you are prepared to recognise anything you might come across in your life.”
The main receptor does the bulk of the work. The secondary receptors can also sense and bind to the foreign adversary; their job is to fine-tune the immune response.
Now we add a key wrinkle: immune cells also need to be able to recognise normal human cells – otherwise we would be destroyed from the inside out.
They do this with the secondary receptors, which look for certain proteins on our cells that mark them as friend, not foe.
One last idea, before we get to CD96. Our immune system is quite effective at hunting and killing cells that become cancerous. But occasionally, a cancerous cell acquires a collection of genetic mutations that cause it to throw up a protein that mimics the ones on a healthy cell.
So our immune cells leave them alone, and they grow and grow into thick tumours.
A drug to melt cancer
In the early 2000s, a small group of scientists, Smyth among them, argued it might be possible to use genetically engineered antibodies to gum up some of the receptors on immune cells – unleashing their destructive power on cancers.
Many scientists were initially sceptical that such a technique could ever work. Smyth was an early believer, and he was right. Checkpoint inhibitors – drugs that unleash the immune system to attack cancer – are one of the great triumphs of 21st-century science.

James Allison and Tasuku Honjo are shown on the screen during the Nobel Prize in Medicine presentation in Stockholm in 2018. Credit: TT News Agency
In 2018, James Allison and Tasuku Honjo were awarded the Nobel Prize for showing how the gumming up of two receptors, CTLA-4 and PD-1, revealed cancer to the immune system.
Smyth dreamt CD96, his lab’s focus, might one day stand alongside the work on CTLA-4 and PD-1 as powerful cancer-busting weapons.
CD96 can bind to a protein called CD155. It shares this ability with two other receptors, TIGIT and CD226.
Scientists first came across it in 2004 as a natural killer cell activator – it seemed to trigger natural killer cell attack.
CD226 seemed to do the same thing, while TIGIT seemed to turn off the attack.
To build a checkpoint inhibitor drug, you need to find and block a receptor that inhibits T cell attack – remember, we’re trying to take the brakes off the immune system. An activator like CD96 is not very useful for this purpose.
Then in 2014, a team including Mark Smyth published a highly influential paper in Nature Immunology.
CD96 wasn’t just an activator, they said. It was a competitor with CD226.
Removing CD96 in mice seemed to allow more CD226 to bind – allowing the immune system to spot and attack cancer.
Scientists often bury the most important lines in a paper right at the end. Here’s the one from the 2014 paper co-authored by Smyth.
“Inhibition of checkpoint molecules on lymphocytes (T cells and NK cells) is proving a useful approach for the treatment of human cancers. Blocking the interaction of CD96 with CD155 may open new opportunities for increasing the recognition of tumor cells.”
Smyth’s team was essentially saying that it might be possible to block CD96 and create a new immune checkpoint drug.
British pharma company GSK took notice. The company filed a patent in 2020 for an antibody that binds to CD96. “The first paper indicating CD96 as a potential immuno oncology target was published by the lab of Professor Mark Smyth in 2014,” the patent reads.
GSK launched a phase 1 human clinical trial of the drug, known as Nelistotug, in 2020. Results are expected later this year.
Does the drug work? We don’t know, as we don’t have the results. The 2014 paper on CD96 has not been retracted, and GSK did a range of its own tests on CD96 that it stands behind.
“Our robust oncology research and development program, including our investigations of Nelistotug in combination with other therapies, is always based on the full breadth of scientific evidence available,” a GSK spokeswoman said.
* Name has been changed to protect the source.
The Examine newsletter explains and analyses science with a rigorous focus on the evidence. Sign up to get it each week.
Read the full article here